(For YEARS, he delivered diapers to our door at a staggering rate. He pushed them inside the front door for me, and once, when I clearly had my hands more than full with 4-week-old twins and a 2-year-old, he offered to unbox them for me. We rewarded him with generous gift cards at the time, and while his deliveries have dropped off dramatically over the years, he still pulls up with a smile and a bounce in his step.)
I am sure I looked puzzled, because I was not expecting anything.
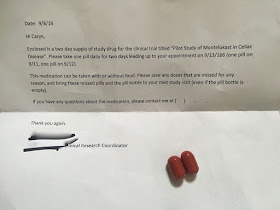
Which was silly, actually, for the clinical trial coordinator had sent me an e-mail on Thursday telling me that she would be "overnighting" me a "2-day supply of study meds," which, of course, meant that I should very much have been expecting some sort of delivery at some point in the day on Friday.
No offense to UPS, but IF had been expecting a delivery driver, I would have been looking for a FedEx truck (in my mind, "overnight" and FedEx are nearly interchangeable words...).
But, in all honesty, I had already forgotten about the delivery I should have been expecting on Friday. To those who don't know me, this might make some question my commitment to the clinical trial, but let me assure anyone who might be concerned that while I am highly ambivalent about this whole journey, I am also absolutely committed.
While a huge part of me is still very much struggling with the fears I have that are associated with participating in something (anything) that is risky (I do, after all, have a husband and three children and a private practice as a social worker...and all sorts of volunteer activities), I still absolutely and completely understand how important it is that subjects in clinical trials remain in the clinical trial for the duration of it whenever possible. Whatever happens, I'm going to see this through.
After the UPS driver left, I looked at the return address on the package. Ahhh. Yes. Of course.
Right.
The Study Drug.
I put the package on the marble table in our foyer. It is the table for incoming and outgoing mail...and anything else that needs to go with us when we leave the house next. Sometimes it is VERY cluttered, but on Friday, the table was empty.
Except for the package.
I left the package there. I knew what was in it, and I knew that I did not need it until Sunday.
I had work to do.
I went back to my home office, but the package drew me down the stairs, back to the marble table.
What if there was something else in the package?
What if there was a note asking me to do something?
What if the study drug required special handling?
What if I had questions?
I opened the package and found a note with simple instructions, and a prescription bottle with my name labeled "Montelukast or Placebo (IRB 15-1413) 10 mg" with a big yellow sticker that read "FOR INVESTIGATIONAL USE ONLY."
Curious, I opened the bottle.
I poured the (two) pills into my hand.
One dose for Sunday, one dose for Monday.
(Gluten Challenge on Tuesday.)
The pills were sort of silly looking -- big, fat, puffy...RED.
I texted a picture to a friend who responded that they looked like "horse pills."
(She's the kind of person who can say this from experience, which gave me pause.)
This morning, I took that first pill.
But first, I hefted it in my hand.
It felt like a pretty regular pill.
Except that it was big.
And then I shook it.
Something rattled around inside.
Very interesting.
It wasn't until after I swallowed it that I realized I could have opened it.
But, I wouldn't have.
And I won't.
Because...curiosity killed the cat...and I don't want any sort of bad karma, even though I know full well that what is in the pill is said and done, and beyond my control.
Whatever happens, I'm going to see this through.
Since my current adventure has little to do with Eating Peanut, but it turns out lots of readers want to follow along, I started Eating Gluten last night. If you want to follow along, you can find it at: Eating Gluten.
Except for the package.
I left the package there. I knew what was in it, and I knew that I did not need it until Sunday.
I had work to do.
I went back to my home office, but the package drew me down the stairs, back to the marble table.
What if there was something else in the package?
What if there was a note asking me to do something?
What if the study drug required special handling?
What if I had questions?
I opened the package and found a note with simple instructions, and a prescription bottle with my name labeled "Montelukast or Placebo (IRB 15-1413) 10 mg" with a big yellow sticker that read "FOR INVESTIGATIONAL USE ONLY."
I poured the (two) pills into my hand.
One dose for Sunday, one dose for Monday.
(Gluten Challenge on Tuesday.)
The pills were sort of silly looking -- big, fat, puffy...RED.
I texted a picture to a friend who responded that they looked like "horse pills."
(She's the kind of person who can say this from experience, which gave me pause.)
This morning, I took that first pill.
But first, I hefted it in my hand.
It felt like a pretty regular pill.
Except that it was big.
And then I shook it.
Something rattled around inside.
Very interesting.
It wasn't until after I swallowed it that I realized I could have opened it.
But, I wouldn't have.
And I won't.
Because...curiosity killed the cat...and I don't want any sort of bad karma, even though I know full well that what is in the pill is said and done, and beyond my control.
Whatever happens, I'm going to see this through.
Since my current adventure has little to do with Eating Peanut, but it turns out lots of readers want to follow along, I started Eating Gluten last night. If you want to follow along, you can find it at: Eating Gluten.